Physiological Barriers
Physiological Barriers
Physiological Barriers to Distribution of Drugs
contains a membrane (or a barrier) with special structural features which can
be a permeability restriction to distribution of drugs to some tissues
Some important simple and specialized physiological barriers are:
1. Simple capillary
endothelial barrier
2. Simple cell
membrane barrier
3. Blood-brain
barrier
4. Blood-CSF barrier
5. Blood- placental
barrier
6. Blood-testis
barrier
1.Simple Capillary Endothelial Barrier:
- All drugs, ionized/unionized, with a molecular size less than 600 Daltons, diffuse through this barrier into the interstitial fluid
- Only drugs bound to blood components are restricted because of large molecular size of the complex
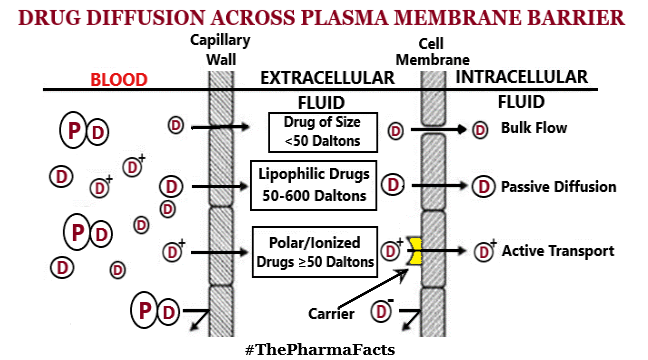
2.Simple Cell Membrane Barrier:
- Simple cell membrane is similar to the lipoidal barrier in the GI absorption of drugs
- The physicochemical properties that influence permeation of drugs across such a barrier are summarized below:
3.Blood-Brain Barrier (BBB):
- Brain capillaries consist of endothelial cells which are joined to one another by continuous tight intercellular junctions comprising of blood-brain barrier as shown below:
- Drugs administered intranasally may diffuse directly into the CNS because of the continuity between submucosal areas of the nose and the subarachnoid space of the olfactory lobe
- Drug may cross to brain via only one of following two pathways:
i) Passive diffusion through the lipoidal barrier having high o/w partition coefficient
ii) Active transport of essential nutrients such as sugars and amino acids. So, structurally similar foreign molecules can penetrate BBB by the same mechanism
- Three different approaches have been utilized successfully to promote crossing the BBB by drugs viz;
i) Use of permeation enhancers such as Dimethyl Sulphoxide (DMSO)
ii) Osmotic disruption of the BBB by infusing internal carotid artery with mannitol
iii) Use of Dihydropyridine Redox System as drug carriers to the brain : CNS enzymes oxidize the Dihydropyridine into Polar Pyridinium Ion form that cannot diffuse back out of the brain, which result in trapping of drug in the CNS
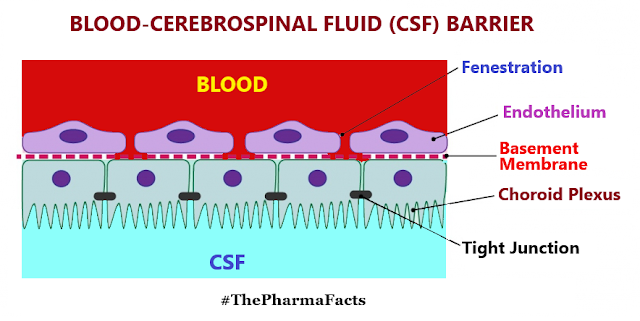
4.Blood-Cerebrospinal Fluid (CSF) Barrier:
- CSF is formed mainly by the choroid plexus of the lateral, third and fourth ventricles
- Choroidal cells are joined to each other by tight junctions forming the blood-CSF barrier which has permeability characteristics similar to that of the BBB
- As in the case of BBB, only highly lipid soluble drugs can cross the blood-CSF barrier with relative ease
- Mechanisms for diffusion of drugs into the CNS and CSF are similar
- Bulk flow of CSF continuously removes the drug & hence drug concentration in brain is always higher than that of CSF [Exception: Sulfamethoxazole and Trimethoprim]
- Maternal and the foetal blood vessels are separated by number of tissue layers made of foetal trophoblast basement membrane and the endothelium which together constitute the placental barrier as shown below:
- Placental barrier has a mean thickness of 25 microns in early pregnancy that reduces to 2 microns at full term without alteration in its effectiveness
- Drugs having molecular weight less than 1000 Daltons and moderate to high lipid solubility e.g. Ethanol, Sulfonamides, Barbiturates, Gaseous anesthetics, Steroids, Narcotic analgesics, Anticonvulsants & some Antibiotics, cross the barrier by simple diffusion
- Placental barrier is not as effective a barrier as BBB or Blood-CSF Barrier
- Nutrients essential for the foetal growth transported by carrier-mediated processes & Immunoglobulins by endocytosis
- Teratogenicity is defined as foetal abnormalities caused by administration of drugs during pregnancy & agent causing this toxic effects is known as Teratogen
- Drugs can affect the foetus at 3 stages as shown below:
- It is always better to avoid all drugs during pregnancy because of uncertainty of their hazardous effects
6.Blood-Testis Barrier:
- This barrier is located at sertoli-sertoli cell junction
- This barrier restricts the passage of drugs to spermatocytes and spermatids
- Preleptotene spermatocytes and spermatogonia are germ cells located outside the blood-testis barrier provided by the Sertoli cells
- Function of this barrier is to hide germ cells present in the adluminal (Near or toward the lumen of a seminiferous tubule) compartment from the circulatory and lymphatic systems & together with local immune suppression, to provide an Immuno-privileged (toleration of antigens without eliciting an inflammatory immune response) microenvironment for the completion of meiosis
Stay tune...
Stay Safe...





Comments
Post a Comment
If you have any query or If you like the post,Please let me know.